Kenya’s plan to produce human vaccines and diagnostics domestically is still coming together.
After meeting Director General Jerome Kim of the International Vaccines Institute (IVI) at Afya House, Health CS Susan Wafula made the announcement.
CEO of the Kenya Biovax Institute Michael Lusiola and Acting Director General for Health Patrick Amoth were also present at the meeting.
In order to produce Covid-19 vaccines and other vaccines, the government has invested between Sh1.5 and Sh2 billion in the Biovax project, according to Wafula.
The main item on the agenda was talking about how the IVI and Kenya’s Biovax Institute will collaborate to make sure Biovax’s mission is accomplished.
Research, partnerships in product development, and capacity building of the local workforce through technical assistance, training, and technology transfers were some of the areas that were investigated.
Kenya officially presented her letter of intent to join the International Vaccine Institute as a state party in Seul, South Korea in November 2022 months prior to the meeting.
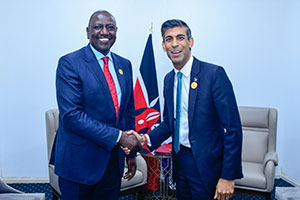
President William Ruto and CS Wafula were present to see the letter being delivered by Foreign Affairs CS Alfred Mutua.
The Kenya Biovax Institute, a government-funded organisation tasked with producing specialised medical goods like vaccines and therapeutics, is about to begin production in earnest.
The first manufacturing facility in Africa to produce messenger RNA (mRNA) vaccines, such as Covid-19 shots, will be established in Kenya by the company Moderna.
The recent shortage of COVID-19 vaccines, which slowed ongoing mass vaccination drives, particularly across many African countries, prompted the decision to expedite the development of a human vaccine facility in the nation.
It is anticipated that the plant will be finished in 2024.
Once finished, the Kenyan manufacturing facility will be the first in Africa to manufacture messenger RNA (mRNA) vaccines, such as Covid-19 shots.
The company plans to invest up to Sh60 billion in the new facility, which will concentrate on producing drug substances for the continent of Africa. The facility may be expanded to include fill-finish and packaging capabilities.