The African Development Fund (ADF) is receiving extra financing from the UK to aid the continent’s communities in developing their economies, generating jobs and enhancing healthcare.
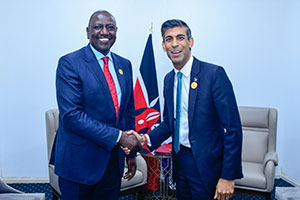
On his first trip to Sub-Saharan Africa since becoming Foreign Secretary, the Foreign Secretary will reaffirm the funding in Kenya as a crucial tenet of the UK’s honest, dependable investment offer.
In a $9 billion overall foreign financing package for the ADF over the next three years, the UK will provide £650 million, giving African nations access to high-impact and affordable financing. Included in this are the £200 million dollars given to the ADF’s new Climate Action Window, which was unveiled during COP27.
With the UK financing, the continent will gain access to power for about 20 million people, better sanitation for over 30 million people, and the creation of over 2.3 million new employment. On the African continent, the fund provides assistance to 37 of the most fragile nations.
Foreign Secretary remarked Working with our friends and allies in Africa is something we appreciate greatly. We all gain from these kinds of connections. The UK provides trustworthy, ethical investment that does not add to debt burdens for nations but instead unleashes enormous potential for economic progress while enhancing global well-being and combating climate change.
The UK’s contribution to the African Development Bank demonstrates our dedication to the region over a lengthy period of time. When we travel together, we shall go far.
In order to assist the growth of the green economy and the creation of jobs throughout Africa, the African Guarantee Fund (AGF) and British International Investment (BII), a UK-based development finance institution, will sign a new risk-sharing agreement.
The arrangement would make $150 million in accessible financing available for small and medium-sized businesses, which is anticipated to enable up to 17,300 loans for companies across Africa. 25% of the loans will be underwritten by BII and 25% by AGF.